Early in my career, I worked with a client—we’ll call her Laura—who was making incredible progress. She was a bright young woman pursuing her degree online, and I was impressed with how motivated and engaged she was.
Then her mother got sick.
Laura was the only one able to care for her mom, so she dropped out of school. She no longer had access to cost-of-living loans, and her financial situation deteriorated significantly.
She kept showing up to therapy, but she stopped making progress. How could she focus on the inner work she was doing when the stress of meeting the needs of her ailing mother (not to mention her own basic needs) weighed on her so heavily?
Laura was one of many clients I’ve had over the years whose therapy progress was significantly impacted by social determinants of health (SDOH). There are likely many more I don’t even know about, because the scope of SDOH is so expansive—ranging from food access to housing stability to caregiving responsibilities.
And I’m not the only clinician who’s ever been in the dark about the undercurrent of SDOH in my sessions. Despite their known impact on therapy progress, SDOH are often overlooked and inadequately documented.
Data gaps like this often inspire our research at Eleos. Our unprecedented access to in-session data allows us to understand unmeasured influences in therapy—including SDOH. For our latest study, we sought to determine how well SDOH are being tracked in mental healthcare. We wanted to understand just how often SDOH come up in therapy—and whether these crucial details make it into the documentation for those sessions.
Our aim was simple: to highlight the gaps so that we, as a profession, can figure out how to close them. By doing so, we hope to help therapists engage clients more effectively—and give providers the data they need to advocate for change on a macro level. Shining a light on these overlooked aspects of behavioral healthcare is our way of pushing for better support of those providing it.
The co-investigators on this study were clinical psychologists Hila Lev-Ari and Chevi Katz, Data Analyst Lee Assenheim, and Director of Data & Research Sam Jefroykin.
What “Social Determinants of Health” Means
“Social determinants of health” is a sociological concept used to describe a wide range of non-medical factors that influence a person’s well-being.
Things like housing stability, finances, education, employment, and caregiving responsibilities are social determinants of health that often impact a client’s experience in therapy—and how well they can engage in, and benefit from, the treatment provided.
For instance, a client who is worried about losing their home might find it hard to focus during therapy sessions, while someone who is juggling multiple jobs to make ends meet may struggle with consistent attendance or engagement in care. In Laura’s case, worry over caregiving responsibilities and financial strain prevented her from progressing toward her therapy goals.
Why We Investigated SDOH Tracking in Behavioral Health
I’m not just a researcher—I’m a therapist, too. I’ve seen way too many clients like Laura come in with a primary health concern—such as anxiety or depression—only to have their progress toward better health hindered by underlying issues related to their social circumstances. It’s a difficult situation for providers to navigate, especially when the resources needed to address social issues are overwhelmingly lacking.
Moreover, these social determinants are not static—they can change over time. A client may start therapy with stable housing, but a few months in, lose their home due to a steep increase in rent. Changes like these can dramatically alter a client’s stress levels and their ability to engage in therapy, but these shifts often are not reflected in the provider’s notes or treatment plans.
Current documentation systems, like electronic health records (EHRs), are partially to blame. If they don’t have a mechanism to prompt, update, or alert providers about SDOH factors and changes, missed opportunities for effective interventions are pretty much unavoidable.
But recognizing and addressing social determinants of health is crucial for effective therapy. Therapists need to understand the full context of a client’s life—beyond the immediate psychological symptoms they present with. A comprehensive approach allows therapists to tailor their interventions more effectively, provide the support clients need to make meaningful progress, and potentially connect them with other resources when available.
Plus, what isn’t measured isn’t managed.
By collecting and analyzing data on social determinants of health, we can not only improve individual client outcomes but also use this information to advocate for systemic changes at both micro and macro levels.
Still, while every therapist I know understands the importance of SDOH, that doesn’t mean they always include it in their session summaries.
Why do clinicians leave social determinants of health out of their notes?
- Time Constraints: With limited time for documentation, therapists might opt to focus on recording immediate symptoms rather than updating SDOH information.
- EHR Limitations: Some systems don’t provide a user-friendly way to update SDOH, making it a hassle for therapists to input relevant information.
- Lack of Standardization: There often are no clear guidelines on when and how to document SDOH changes, leading to inconsistent reporting of these factors.
- Uncertainty About Next Steps: Even when therapists have the time to identify and report changes in SDOH, many—including myself—experience a sense of learned helplessness. We’re unsure if our organization has the resources to address worsening SDOH, which can discourage thorough documentation of these factors.
How We Conducted the Study
To understand how well SDOH are being tracked in mental healthcare, we designed a comprehensive study that began with manually reviewing 100 random therapy sessions—without the support of Eleos—to identify the presence of SDOH topics. Each session was broken down into micro-dialogues, which are the key moments where therapists and clients discuss specific topics.
Our team of clinical experts meticulously analyzed and coded these sessions to identify any discussions involving social determinants of health.
We ended up reviewing 1,762 micro-dialogues, noting the frequency at which SDOH factors were mentioned and whether they were included in the corresponding progress notes.
This allowed us to quantify how often SDOH topics were discussed during therapy sessions versus how often they were documented—ultimately revealing a clear picture of the gaps in current documentation practices.
The Prevalence of SDOH in Behavioral Health: What We Found
Our study revealed some noteworthy insights into how social determinants of health are handled in therapy sessions and progress notes:
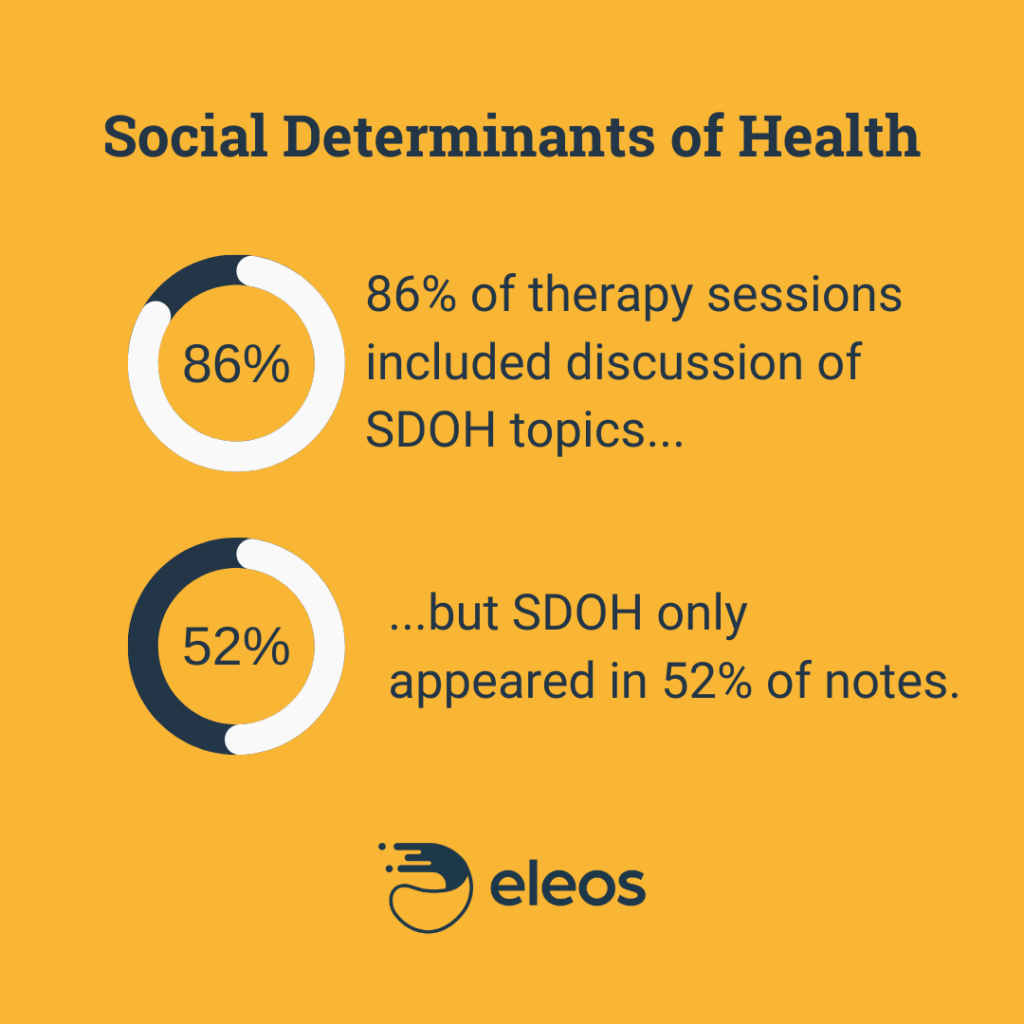
86% of sessions included discussion of at least one SDOH topic.
This was a positive finding—therapists are indeed aware of and actively addressing SDOH factors during sessions.
Only 52% of progress notes documented these discussions.
This gap is concerning. It means that nearly half of critical SDOH discussions are not making it into official client records, potentially leading to missed opportunities for effective follow-up and intervention.
Significant SDOH factors are underreported.
We found that important topics like neighborhood environment and education were underreported in client documentation. For instance, clients mentioned things like realizing they should move out of their apartment due to their roommate’s drug use or dropping out of school to care for a family member—but these issues were not documented.
These findings have important implications for client care. When social determinants of health are not adequately documented, it limits a provider’s ability to tailor interventions effectively over the entire course of care. Additionally, if a different provider takes over (because, for example, the original provider leaves the organization), gaps in documentation will almost certainly disrupt the continuity of care. Omitting SDOH from documentation also hinders our ability to address and advocate for these issues at the system level to effect change at scale.
How Eleos Can Help Providers Better Document SDOH
Timely and Intuitive Documentation
At Eleos, we’re making a big impact on the way therapists document social determinants of health (SDOH). Our AI technology is designed to analyze sessions and identify important topics, including SDOH, as they come up in real time. Those themes are then incorporated into our AI-generated note suggestions—meaning crucial factors like housing stability, financial stress, and caregiving responsibilities can be documented in a timely manner without any extra effort from the therapist.
Care Quality and Continuity
Automatically incorporating SDOH into client documentation unlocks a host of far-reaching benefits, including:
- Improved Note Accuracy: Eleos captures details that might be missed or forgotten with manual note-taking. That way, providers can document all relevant information so current and future members of the care team have a full understanding of the client’s situation.
- Timely Updates: With Eleos, 90% of notes are submitted within 24 hours of service—which means updates to SDOH factors are recorded almost immediately after they are discussed. When changes in a client’s circumstances are documented right away, treatment plans can be more responsive.
- Better Client Outcomes: When providers have up-to-date information on a client’s SDOH factors, they can tailor interventions and therapy plans more effectively. In addition to supporting better outcomes for clients, SDOH data tracking and analysis helps us identify global trends and patterns, which can then help inform advocacy efforts and treatment protocols.
Where We Go From Here: The Future SDOH, Behavioral Health Documentation, and AI
I see immense potential for AI to revolutionize how we handle SDOH in mental healthcare. My vision is to create a future where AI not only assists in documenting these crucial factors on a micro level, but also provides actionable insights that help organizations address them more effectively on a macro level.
Imagine an AI tool that not only flags a client’s financial difficulties, but also suggests potential resources or interventions based on similar cases. Or, an AI tool that alerts therapists to subtle changes in a client’s social environment that may impact their mental health. This level of support would empower therapists to manage SDOH more proactively and comprehensively, leading to a higher standard of care.
But we’ve got a long way to go.
With only 50% of therapists currently documenting the SDOH factors that impact their clients’ therapy progress, we don’t have nearly enough data to begin tackling the issues SDOH represents—at the individual, organizational, or societal levels.
This study is just the first step. It highlights the gaps and sets the stage for necessary changes in our documentation practices. With Eleos, we aim to bridge this gap, ensuring that these critical factors are never overlooked or under-documented again. By leveraging AI, we can pave the way for a more holistic and effective approach to mental health treatment—one where we can make sure every client’s story is fully told and their needs fully met.

