The landscape of behavioral health reimbursement in California is on the cusp of a significant transformation.
Most providers in the Golden State are already familiar with the California Advancing and Innovating Medi-Cal (CalAIM) program, an initiative designed to impact everything from care delivery and documentation to payment models.
Many therapists are celebrating the changes that have been implemented thus far, which have reduced documentation requirements for behavioral health services to only the essentials, easing administrative burdens.
But now, a more complicated part of CalAIM—the sweeping payment reform— is taking effect July 1, 2023.
Designed to revamp and enhance the Medi-Cal healthcare system, this reform promises improved patient outcomes in the long term. But it also casts a shadow of financial uncertainty and pressure for behavioral health providers in the near term.
The good news?
With CareOps Automation technology like Eleos Health, providers can smoothly navigate these changes while maintaining—and even improving—care quality.
From Interim Payment to Value-Based Care: The CalAIM Transition
Historically, Medi-Cal paid counties on a cost-based reimbursement basis. Counties claimed payment on an interim fee-for-service basis, followed by a thorough audit, reconciliation, and cost settlement process. CalAIM, however, is designed to shift this system to a value-based model.
As a preliminary step in the transition to a full value-based model, County Behavioral Health (BH) plans are now required to claim fee-for-service reimbursement at fixed rates. This creates real-time visibility into exactly what services are being performed and at what cost—opening the door for future efforts to optimize care efficiency and reduce waste.
The transition to value-based care via CalAIM can be broken into three main phases, as noted in this resource:
- Cost Reconciliation (Where We Are Now): Services are reimbursed at a provisional rate and later reconciled with costs during a settlement process that can take several years.
- Fee-for-Service (Where We Will Be with the July 1 Changes): Services are reimbursed at a fixed rate with no cost reconciliation or settlement.
- Value-Based Care (Where We Are Going in the Future): Services are reimbursed according to risk-based incentive models designed to drive improvements in overall care quality, patient outcomes, population health, service efficiency, and cost management.
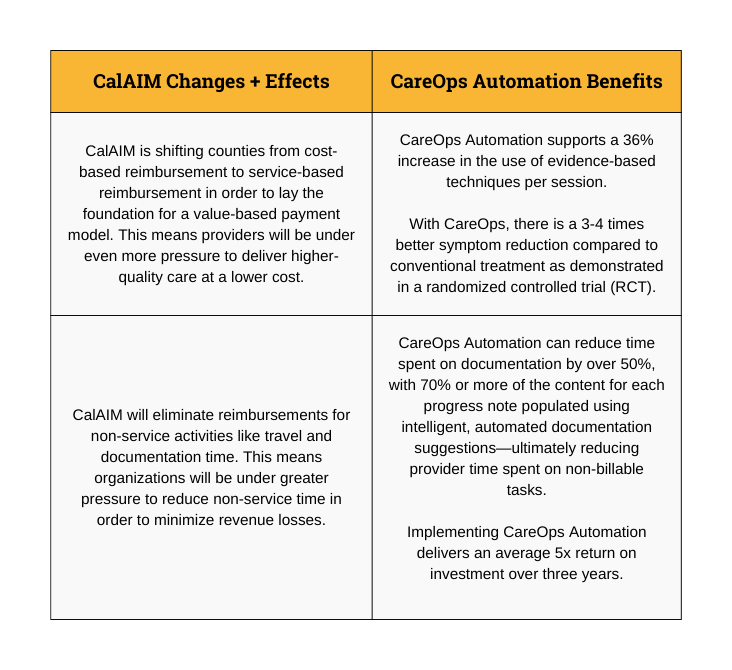
Although the July 1 changes represent a crucial first step toward implementing a true value-based care model, they also present distinct challenges for providers—especially when it comes to tracking evidence-based care and managing time spent on non-service related tasks.
Here’s a quick breakdown of those changes, the challenges they pose, and how a CareOps Automation platform like Eleos can help. You can also click here to download a one-page overview.
Closing the Gap: CareOps Automation to the Rescue
Per the CalAIM reform, providers will no longer receive reimbursement for travel and documentation time. CareOps Automation can help providers tackle this challenge effectively. Augmented intelligence technology reduces time spent on documentation by 50%, with over 70% of note content being automatically generated via highly-accurate machine learning models that are purpose-built for behavioral health and trained by clinical experts. This means providers can redirect their time and focus toward delivering superior patient care in ways that will be reimbursed under the new system.
To prepare for the transition to value-based reimbursement, developing an efficient system to track evidence-based care becomes a top priority. With CareOps Automation, providers can significantly advance their capabilities with automatic tracking of evidence-based techniques used in sessions as well as a variety of other key metrics on care delivery..
This technology has been shown to support a 35% increase in the use of evidence-based techniques per session—a possible result of regular objective feedback on skills used during sessions. According to a randomized controlled trial, it also doubles client engagement and enables 3-4 times better symptom reduction compared to conventional treatment—critical markers of value-based care.
Further, CareOps Automation also allows providers to streamline outcomes tracking, generate vital insights about patient progress, and facilitate tailored provider supervision and training. These advantages lead to better care at a lower cost—a driving force behind healthcare payment reform under the CalAIM initiative.
ROI and the Promise of Better Care with CareOps Automation
CalAIM reform is driving a transformative shift toward value-based care and improved patient outcomes. Providers can confidently embrace this change with CareOps Automation, a solution that aligns perfectly with CalAIM’s objectives, offering enhanced care and a 5x average return on investment (ROI) within three years.
CareOps Automation, powered by advanced AI technology, streamlines workflows, reduces administrative burdens, and optimizes resource utilization. It provides a seamless ally to providers as they navigate the demands of CalAIM, allowing them to deliver exceptional patient care while ensuring long-term financial sustainability.
The synergy between CareOps Automation and CalAIM points to a future with better behavioral healthcare and less burden on clinicians. Let CareOps Automation empower your organization to create a better system for clinicians and patients alike.
Click here to download a quick one-page overview of the CalAIM payment reform and how Eleos can help.
For more insights into our platform’s capabilities and its transformative impact, explore our related blog posts, case studies, and video testimonials that demonstrate how Eleos Health delivers documentation time savings, improved care quality, and impressive ROI.
