That healthcare requires clinical evidence to support its effectiveness is a well-established principle in physical healthcare. No one would use a treatment or medication that had not been rigorously tested and peer-reviewed. However, in the behavioral health arena, this same standard is not found.
There is a growing movement to attempt to apply the same empirical standards to behavioral health for the benefit of clients, clinicians, and healthcare systems.
What is evidence-based behavioral healthcare?
Evidence-based care is based on data that has been empirically demonstrated to have a measurable effect. The key aspect here is the ability to prove and replicate the same results. All clinicians working within the field are using methods that they understand to be effective and bring value to their clients. As new methods are developed, their initiators make efforts to document and define their process. However, success in one setting does not necessarily lead to success in other settings or when the same techniques are applied by clinicians of varied levels of experience.
For a behavioral health intervention to be empirically demonstrated to produce results, it must be tested with the same rigor as you would expect from other clinical trials. For this to be the case, it must be subject to controlled testing to demonstrate its efficacy.
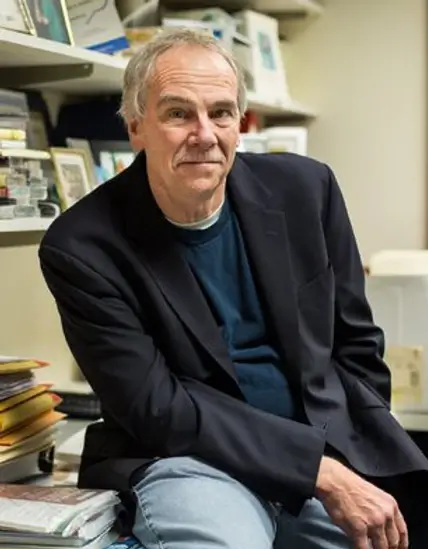
Dr. Steven D. Hollon, the winner of the American Psychological Association Award for Distinguished Scientific Applications of Psychology, is a longtime advocate of applying an evidence-based approach to behavioral healthcare. He explains, “We test medications to demonstrate that they are safe and effective. We should be applying the same standards to behavioral health.”
What is being measured?
For a therapeutic method to be ‘evidence-based’ it must demonstrate measurable results in a particular area. As Dr. Hollon notes, ‘Most approaches work better than doing nothing. Our goal is to define which approach has a specific impact.” By comparing one form of intervention with another, clinicians are able to select the treatment modality that will have the maximum impact for a particular condition.
‘Most approaches work better than doing nothing. Our goal is to define which approach has a specific impact.’
Dr. Hollon
In the case of depression, a number of studies have compared outcomes with behavioral health interventions with pharmaceutical treatments. The positive results of these studies have created a general consensus that empirically supported psychological treatments can have a major impact, at least on par with medication in the short-term and being more enduring in the long term.
It is important that standardized measurements be applied to behavioral health practices to monitor the efficacy of care, both in terms of determining which techniques are most applicable and for monitoring recovery in general.
Why does evidence-based care matter?
The American Psychological Association identifies that clinicians have a dual responsibility to both ‘ensure that individuals are treated according to best practices and to reduce unnecessary expenditures’ as the healthcare system is overtaxed with ever-rising costs.
Dr. Hollon comments, “Payers have an interest in providing clients with the most cost-effective treatment. When we can demonstrate that psychological interventions can offer greater promise for long term recovery than medications, then payers are more likely to cover those interventions.”
“Payers have an interest in providing clients with the most cost-effective treatment. When we can demonstrate that psychological interventions can offer greater promise for long term recovery than medications, then payers are more likely to cover those interventions.”
Dr. Hollon
Testing and defining evidence-based methods of behavioral healthcare brings clients the benefit of modalities of care that are best placed to help improve their situation and greater access to those modalities by generating a greater willingness on the behalf of payers to cover that care.
Implementing evidence-based care internationally
The advantages of applying evidence-based care have been recognized by governments around the world. Great Britain has a particularly robust system for creating national guidelines around behavioral health treatments. Since 2004, the National Institute for Health and Care Excellence (NICE) has systematically reviewed the evidence for the effectiveness of a variety of interventions. The results of these reviews were used in the creation and publication of a series of clinical guidelines.
Dr. Hollon explains, “The NICE committee brings together experts from different fields of behavioral health to review the data. This ensures a balance among the committee. If they are reviewing a study on CBT interventions, those clinicians who specialize in other areas will offset any inadvertent bias towards CBT that the CBT practitioners on the committee might have.”
However, once the best practice guidelines were established, it became apparent that there was a lack of trained clinicians to implement them. Therefore, the NICE guidelines have been used as the base for a large-scale training program, the Improving Access to Psychological Therapies (IAPT) program. IAPT aims to train over 10,500 new psychological therapists and deploy them for the treatment of depression and anxiety disorders.
The importance of measuring outcomes
A key aspect of the IAPT program is measuring outcomes. Inherent in the process of applying evidence-based care is the collection of data. This process is not only a function of clinical trials. It is important that clinicians collect data on client outcomes throughout the therapy process to correct, gauge and tailor their interventions.

IAPT currently treats over 560,000 members annually and collects clinical outcome data from 98.5%. This provides an invaluable sight into their experiences and the efficacy of treatment methods. The information is collected by IAPT throughout the treatment process. They found that many existing programs overestimated their own effectiveness as they only collected feedback when treatment ended. As many clients end therapy without warning, their feedback was not collected.
“Clients who drop out of therapy are likely to have had a less positive experience than those who complete their assigned program,” Dr. Hollon explains.
“If you only collect client outcomes at the end of treatment, your statistics are likely to be skewed towards those who were happy with their experiences. Therefore, it’s very important that you collect outcomes on an ongoing basis.”
Dr. Hollon
How automation can make practicing evidence-based care easier
One of the challenges in practicing evidence-based care is collecting the necessary data on client outcomes to use as a basis for future decision making. The Eleos system was designed as the next generation in workflow support tools for behavioral health clinicians. Using secure therapy-specific voice analysis, Eleos provides clinicians with actionable insights into the therapy session while also providing an automated compliance-ready progress note. This gives clinicians insight into in-session trends. Between sessions client- reported outcomes are also collected which enables clinicians to have a full picture of their client’s progress.
By applying the same rigorous standards of empirical support behind behavioral health methodologies as found in other areas of healthcare, clinicians can offer their clients a proven path to recovery. This includes applying an ongoing assessment of client outcomes during the course of treatment. Both clients, clinicians, and healthcare systems stand to benefit from the improved outcomes and resulting cost-savings that can be found in applying evidence-based care.
