Everyone knows the pandemic forced wider adoption of all things digital. While the jury’s still out on some of the technological mainstays resulting from that shift—lookin’ at you, QR code menus—the benefits of many now-ubiquitous conveniences are hard to ignore.
In the healthcare space—particularly behavioral health—technology has flourished in the wake of long-gone social distancing requirements.
Pre-pandemic, only 10% of mental health professionals regularly used technology in their sessions. Now, a staggering 80% rely on it for the majority, if not all, of their practice.
But there’s still a significant gap between the education mental health clinicians receive in graduate school and the technology-heavy practice environments they’re entering upon graduation.
That’s the topic of a new research paper highlighting the urgent need for specialized curriculum in digital mental health tools (DMHT). With today’s providers relying more on technology in everyday practice, graduate programs must evolve to teach students how to integrate these tools into the care process effectively and responsibly.
We sat down with one of the study’s lead researchers, Dr. Josef Ruzek, to discuss this paper’s exploration of one such training program at Palo Alto University. The former Director of the Dissemination and Training Division of the U.S. Department of Veterans Affairs National Center for PTSD, Dr. Ruzek has long been a proponent of leveraging technology to enhance care, and he’s bullish on the possibilities it brings for both access and efficacy. Lack of training, however, is a major barrier to realizing that potential.
“One of the reasons why mental health professionals should integrate technology is that we believe it will improve clinical outcomes,” Dr. Ruzek said in a recent interview with Eleos. “There’s a lot of evidence now that web-based programs for all kinds of disorders can be very effective—even as effective as face-to-face care, if done well. But clinical psychologists, psychiatrists, social workers, and others are not actively trained on how to use these technologies. Most graduate training programs don’t incorporate any kind of course or specialized planning for how to do this. At Palo Alto University, we thought we should get out in front of this and try to create a model clinic to help them do that.”
Bringing Therapy Curriculum into the Digital Age
The sudden pivot to tech-driven care was also a sharp about-face for best practices in care delivery.
As Dr. Ruzek reflected, “[Clinicians] had fallen into a conventional set of ideas that [technology] is bad—that we shouldn’t do it. But when COVID hit, it pushed all the systems so everybody went to it all at once. Otherwise, there would have been no care. And now that COVID has wound down, almost all of those services have retained their use of these technologies.”
This sudden transformation exposed a gap in mental health: the lack of formal training on how to properly use DMHT in therapy practice. As the paper explains, that’s exactly what drove Palo Alto University to create their revolutionary eClinic.
“We just thought, ‘Let’s try to create a clinic that is a laboratory where we can [train students in DMHT] and work out some of the training content,’” Dr. Ruzek explained.
The eClinic at Palo Alto University gives graduate students in mental health the opportunity to use technology as a core component of their clinical training.
“We wanted to make it a course so that we could cover the range of related topics that are important…and help people incorporate the tools in the care,” Dr. Ruzek said.
Establishing Standards for Digital Mental Health Training
Nestled within the broader context of a counseling and psychology graduate program, the PAU eClinic merges digital tools with therapeutic care to create standards around this new format for practice. The fully online clinic not only serves a diverse population across California, but also functions as an integral practicum for advanced graduate students.
eClinic Curriculum Components
Students engage with the eClinic in three stages.
- Asynchronous Onboarding: This segment introduces students to DMHT through online courses, laying the groundwork for their practical training.
- Didactic Curriculum: Implemented via monthly seminars, this curriculum covers a range of topics from the logistics of actual tech usage to ethical considerations and HIPAA compliance—all led by experts in the field.
- Ongoing Supervision: Students receive weekly guidance from licensed supervisors, integrating their learning with real-world applications.
Certificate in Digital Mental Health
To formalize their training, students complete a certificate program encompassing four key areas:
- Foundations of Digital Mental Health
- Suicide, Risk Assessment, & Treatment Planning via Tele-Mental Health
- Evidence-Based Internet Interventions to Reduce Health Disparities
- Technology and Mental Health for Children and Adolescents
These courses, providing both contact-hour credit and continuing education units, offer an in-depth exploration of digital therapy, its benefits, and the practicalities of integrating technology into mental health care.
Skills Development Seminars
Seminars allow students in PAU’s program to interact directly with digital tools and develop specific technology-related clinical skills. These tools include everything from self-monitoring apps and virtual reality (VR) programs to synchronous and asynchronous telemental health delivery systems.
Strategies for Digital Tech Evaluation
Technology changes fast, and new tools are always emerging. To help mental health professionals keep pace with the speed of innovation, the program provides the following guidelines for evaluating future technologies:
- Evidence-Based Effectiveness: How well does the technology work in practice?
- User Engagement: Is the technology engaging enough to keep clients committed?
- Privacy and Security: Does the technology meet legal and ethical standards for client confidentiality?
- User Experience: Is the technology accessible and easy to use for clients?
Integrating Eleos Health into Therapy Education and Practice
Eleos Health’s technology is at the center of every therapy session conducted within the eClinic. Dr. Ruzek says that choice was very intentional—and reflective of the value Eleos offers as a clinical support tool.
Clinical Analysis in the Classroom
Dr. Ruzek pointed specifically to the Eleos platform’s clinical analysis capabilities—including its ability to identify therapy themes and interventions—as a value-add for PAU’s graduate program.
“It’s been amazing to incorporate Eleos because it has these features in it that are extremely important for the field,” Dr. Ruzek said, pointing specifically to the platform’s ability to track and analyze data on therapy interventions, themes, and progress. “It’s a lot better to have this administered through a platform like Eleos, which makes it more organic to the process—and it reduces the work, especially for the therapist who can bring up the dashboard and look at it. And it also makes it more convenient for the client.”
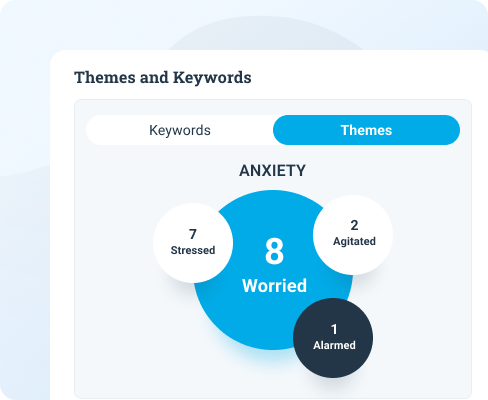 |  |
A Fresh Approach to Supervision and Training
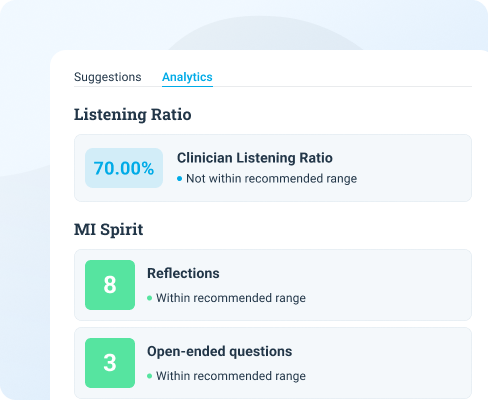
Eleos Health revolutionizes not just how therapy is delivered, but also how it’s supervised and refined—something that’s especially valuable in the context of graduate-level training. The ability to record, transcribe, and analyze sessions offers a previously unimagined level of insight into the therapeutic process. It also gives supervisors tangible data to guide their feedback, moving supervision from a subjective process to an objective, evidence-based one.
A New Paradigm for Therapy
The eClinic’s use of Eleos is a leap forward for mental health training and care. The data analytics dashboard presents each therapist’s work in a new light, offering clear metrics for evaluation, reflection, and improvement. And the Eleos platform’s focus on tracking engagement, such as therapist-versus-client talk time, directly supports PAU’s goal of fostering effective, active, tech-powered mental health care.
The goal of any clinical education program is to prepare students for the realities of practice—and in this day and age, that includes the use of innovative technology. While this paper offers a glimpse into how program administrators can accomplish that, more widespread integration of technology in therapy curriculum is needed—not only to keep graduating providers on the leading edge of innovation, but also to further the innovation care itself.

