Pre COVID, 46.6M American adults struggled with a behavioral health condition; these numbers have now spiked. We are talking about one in three adults in the U.S. who have reported symptoms of anxiety or depressive disorder during the pandemic. We are in a national behavioral health crisis.
Clearly, the pandemic has pushed the demand for behavioral health services to an all-time high. At the very start of the pandemic, we’ve pointed out the various challenges now arising for behavioral care, with the focus on access to care, quality of care, and administrative overload. Unfortunately, if you are one of the millions currently in need and are looking for a professional to talk to, you will likely have to wait. Length of wait…unknown.
Even prior to the pandemic and this tsunami of demand, we had a massive shortage in behavioral health clinicians on hand. According to the Department of Health & Human Services data, back in 2013, we had a shortage of 208,660 clinicians. However, a new report issued 3 weeks ago by SAMHSA (The Substance Abuse and Mental Health Services Administration) shows that today 4.5M more behavioral health professionals are needed, a shortage of around 87%!
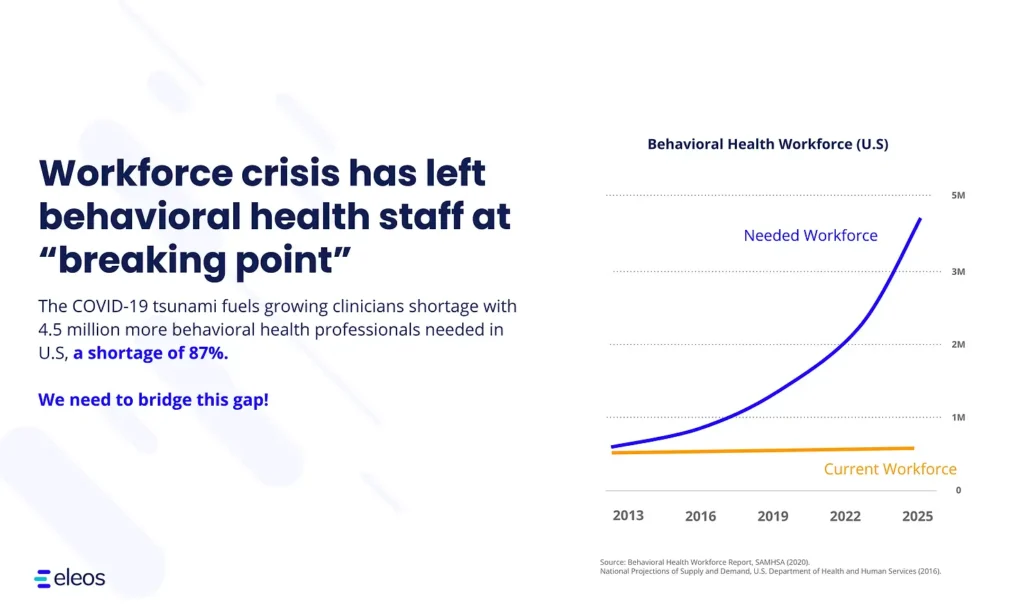
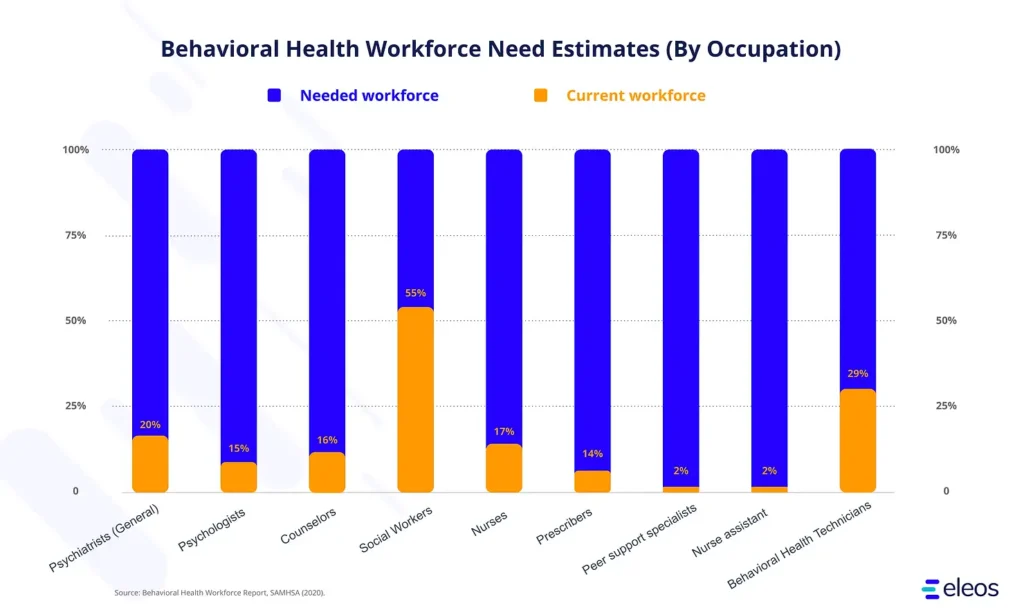
The sad reality is that any of us who may want to get the help we need, want to get it right away, but what clinician will guide us on our journey so our healing can take place? The demand has increased exponentially while supply has stayed flat and creating a few million newly available clinicians will take time.
We see a need for a bottleneck new opening to allow greater access to quality behavioral care. One of the main challenges we are facing is that clinicians spend, on average, 35% of their time in the documentation of patient data. In real-world terms, clinicians were found to spend an average of 16 minutes and 14 seconds on documentation for every patient encounter. If we were to cut this time significantly, it is fair to estimate that even a small portion of the freed-up time, on a national level, can dramatically help improve access to care.
What can we do now?
We believe that in today’s world of mental and behavioral health, Artificial Intelligence (AI) is opening up new possibilities and capabilities for psychotherapists and other mental health professionals. AI and other novel technologies have shown promising results in other healthcare verticals (such as radiology and pathology). It is time to leverage these innovative technologies and apply them in behavioral and mental health daily practice.
For example, Natural Language Processing (NLP) and Natural Language Understanding (NLU), a subset of AI, have made it possible to surface actionable clinical insights that dramatically improve treatment outcomes and help clients get better, faster. In addition, it enables the clinician to automatically generates progress notes based solely on the verbal exchange between a client and a clinician with no typing by the two. Eleos Health, the leader in powering the future of behavioral health, has shown that one can achieve a 42% reduction in time spent on progress notes writing.
It is evident we need to close this growing gap and empower our clinicians’ workflows so they can focus on what matters most, caring for their clients.
