Note: This is the second article in a two-part series exploring GRAND Mental Health’s success with the CCBHC model of care. Check out part one here.
Community mental health clinics grapple with a lot of challenges: limited funding, high caseloads, and a rapidly changing landscape are just the tip of the iceberg. At GRAND Mental Health in Oklahoma, though, these aren’t merely hurdles to overcome—they’re catalysts for innovation.
By embracing the Certified Community Behavioral Health Clinic (CCBHC) model, GRAND is not only transforming its own care approach, but also helping to reshape mental healthcare across the nation.
Discovering the CCBHC Model
Certified Community Behavioral Health Clinics (CCBHCs) have emerged as a key response to the complexities and unique needs of mental health treatment in the 21st century. These centers embody a new way of delivering services, focusing on comprehensive, community-centered care that addresses both mental and physical health needs. CCBHCs strive to make treatment more inclusive and accessible, breaking down barriers and ensuring that anyone—regardless of their financial situation—receives the care they need.
CCBHCs operate under standards designed to ensure the highest level of care. These include:
- offering a broad range of mental health and substance use disorder services;
- providing 24/7 crisis care;
- integrating additional health services to address physical health needs;
- tailoring services to fit the unique needs of the community; and
- catering to various age groups, cultures, and subpopulations.
This flexibility makes CCBHCs invaluable in addressing overlooked or underserved needs within a community.
GRAND Mental Health is a sterling example of the CCBHC model in action. Located in Oklahoma, GRAND’s CCBHC journey involved more than an adjustment in operations; it redefined their entire approach to care. Embracing the CCBHC model allowed GRAND to transcend the traditional care delivery process, enabling the provision of more holistic and integrated mental health services—and exemplifying the transformative potential of the CCBHC model.
Fusing Mental Health Ethos with Startup Agility
GRAND Mental Health found success in combining two seemingly incompatible worlds: the nimble agility of startup culture and the mission-driven foundation of mental health practices. After reaffirming their commitment to their mental health mission and ethos, they integrated principles typically used in tech startup environments to foster innovation, agility, and resilience.
“It’s just applying a philosophy of starting at the end—what is the outcome that we’re looking for? Then [it’s] working our way backwards and applying all available resources, laser-focused on the end goal until we accomplish it. And then we continually monitor what we need to change, because it’s all a hypothesis and we have to adjust that over time.”
– Josh Cantwell, COO of GRAND Mental Health

Josh Cantwell, the COO of GRAND Mental Health, highlighted three underlying principles of this philosophy:
1. VISION: Setting the Destination
By clearly defining outcomes—such as limiting patient hospitalizations to only the most severe cases—GRAND created a guiding star to illuminate their path forward. Cantwell pointed to three sub-steps for setting a vision:
- Define Clear Outcomes: Focus on tangible goals, such as reducing unnecessary hospitalizations.
- Embrace a Guiding Philosophy: Let the desired outcome guide every decision—clinical or administrative.
- Take a Holistic Approach: Ensure decisions resonate with the larger mission of mental health well-being.
2. INNOVATION: Building the Solution
Embracing the spirit of startup innovation, GRAND was unafraid to challenge traditional structures. Here’s how they put that spirit into action:
- Question Conventional Roles: Introduce roles like the Integrated Team Manager—a therapist who also manages a small team of behavioral health support specialists—to optimize resources.
- Deploy Resources Strategically: Use specialized skills, like MBAs, where they are most effective.
- Incentivize Creatively: Offer unique benefits, such as wellness days, to foster a committed and healthy workforce.
3. ITERATION: Refining for Excellence
GRAND constantly evaluates and adjusts its strategies. Their mantra: Treat every strategy as a hypothesis. If it doesn’t end up aligning with goals, shift and adapt. This means:
- Test and Pivot: If an approach doesn’t work, adjust and move forward.
- Fail Fast: Learn quickly from missteps, allowing for rapid course corrections.
- Maintain a Continuous Feedback Loop: Encourage regular evaluations to refine strategies and ensure alignment with core goals.
“I tell [our CEO] Larry that it looks like he hasn’t made a bad decision since 2015. But we’re just applying these principles. Whatever decision we make, we’re failing fast, and continually changing our approaches until they’re meeting our needs.”
– Josh Cantwell, COO of GRAND Mental Health
There is no doubt that GRAND’s innovative approach is highly effective. After setting out to reduce psychiatric hospitalizations, they implemented, reviewed, and revised their model until they started seeing the impact they desired. The result was a 93% decrease in psychiatric hospitalizations in Oklahoma.
These experiences offer a valuable template for other CCBHCs—and really any behavioral health organization—by demonstrating that it is possible to sustain rapid growth and expansion while staying true to core mental health ethics. The secret lies in combining the best aspects of two different worlds, staying open to innovation while always keeping client welfare at the forefront.
Investing in Data Reporting and Management
On the topic of data reporting, Cantwell explained that GRAND Mental Health invested heavily in data collection and management systems. They recognized that a robust and agile data infrastructure is fundamental to building cost reports—and thus, collecting cost reimbursement in the CCBHC model. (For more on the payment model GRAND adopted as part of their CCBHC transformation, check out part one of this series.)
Their process for data collection needed to be comprehensive and flexible, allowing for potential retrospective reviews. It had to be capable of logging all aspects of their operations, even data points that didn’t seem immediately useful. In essence, they believe there are no wasted data points.
Cantwell also highlighted the importance of having the right leadership involved in data management. Agility in managing data is critical—and data teams should work in iterative cycles to produce small pieces of usable information. This allows the organization to build on initial data pieces rather than waiting for a perfect product—which might not end up meeting their needs, thus requiring them to go back to the drawing board.
8 Quick Tips on Data Management from GRAND Mental Health
- Invest in Data Infrastructure: Recognize the significance of agile data systems, especially for cost reports and reimbursement processes.
- Ensure Comprehensive Collection: Data collection should be all-encompassing and adaptable, allowing for potential retrospective reviews.
- Waste Nothing: Embrace the belief that all data points, even seemingly unimportant ones, hold value.
- Build a Strong Leadership Team: Prioritize having the right leadership in place for data management to guide and direct the process.
- Take an Agile Approach: Encourage data teams to work in iterative cycles, producing bite-sized chunks of actionable information.
- Prioritize Outcome-Driven Care: Always validate the care model with tangible outcomes. The end goal is to improve lives, and operations should be evaluated accordingly.
- Enable Flexibility in Treatment: Focus on individual improvement and tailor treatment plans to ensure optimal results for each patient.
- Embrace Change and Innovation: Every challenge is an opportunity. Emphasize the importance of embracing change, making astute data management investments, and centering efforts on people’s well-being.
A key point Cantwell stressed is that the care model at GRAND always has to be validated by outcomes. The ultimate goal is to improve people’s lives. That’s why their operations need to be measured based on care effectiveness—and the data points they collect need to reflect that.
He also shared a personal anecdote illustrating GRAND’s approach to patient treatment and how outcomes data can help shape more effective treatment strategies. Early in his career, Cantwell used a fairly rigid framework for treating depression. Over time, though, he realized that this approach was not sustainable; it didn’t allow enough flexibility to address the unique needs and rate of progress for each individual client. This experience represents how GRAND Mental Health now approaches patient treatment—focusing on individual improvement and using data to personalize treatment plans with the goal of ensuring the best possible outcome for each person.
Leveraging Technology and Looking Forward
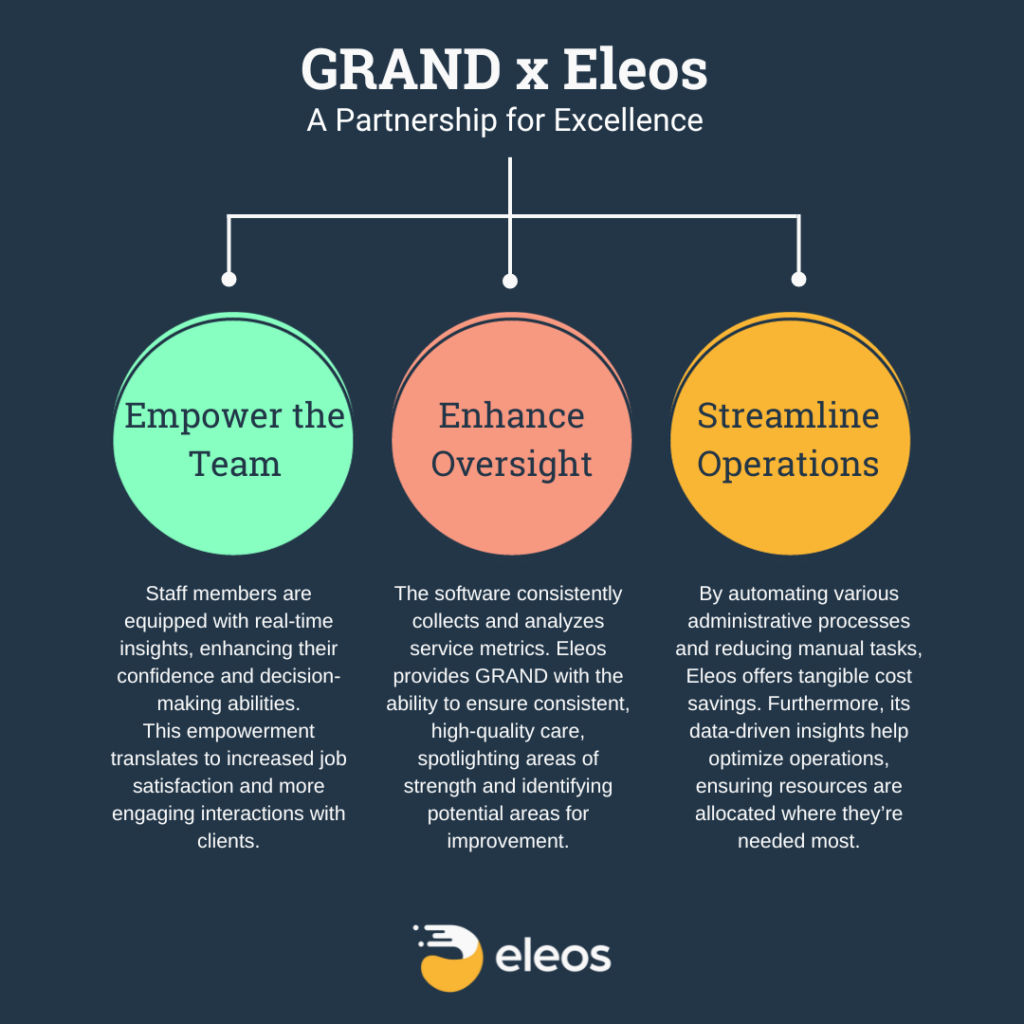
As Cantwell looks to the future—and even reflects on the present—technology like Eleos Health plays a central role. The benefit of CareOps Automation software like Eleos is threefold: a gift to the staff, a tool for better service monitoring, and a mechanism for increased efficiency and cost savings.
Since implementing Eleos, Cantwell says GRAND has improved staff engagement and work processes significantly. The Augmented Intelligence tools Eleos provides help align workload expectations between management and staff by creating a common language for discussing job requirements and performance. Furthermore, the technology allows staff to finish their case notes immediately after their sessions, freeing up their time and potentially enabling them to provide more services.
Apart from boosting staff efficiency, Eleos also offers unique monitoring capabilities. It allows the organization to assess whether evidence-based modalities are utilized appropriately in sessions—without the need for a third-party observer. This ultimately enhances the quality of care provided. GRAND places a high priority on outcomes, making Eleos a crucial partner in making sure every client gets the best possible care.
But Eleos isn’t just some trendy tool—it’s an innovative technology that is essential to keeping pace with the rest of the healthcare world.
“This is not the future; this is the present. This isn’t even us being ahead. This is one of those things that’s just keeping us level with the rest of the playing field.”
– Josh Cantwell, COO of GRAND Mental Health
Cantwell believes that in two years’ time, behavioral health organizations not leveraging AI will fall behind. So, he says Eleos will continue to play a key role in reinforcing GRAND’s position at the forefront of the mental health sector.
Expanding GRAND’s Impact
In looking to the future, GRAND expects to keep expanding while holding tight to their core goal of increasing access to mental health services. The organization firmly believes that serving more individuals at the early stages of their mental health journey reduces their likelihood of escalating to severe mental illnesses, multiple crisis episodes, or even suicides.
GRAND Mental Health’s innovative approach to mental healthcare—from embracing the CCBHC model to merging the startup mindset with a compassionate mission—offers a blueprint for other CCBHCs. Their insights and lessons learned emphasize the transformative potential of agility, innovation, and a relentless focus on improving lives.
Interested in learning more about all the ways Eleos can support your organization’s CCBHC journey? Get in touch with our team now.
And stay tuned to the Eleos Health Blog for more insights and wisdom from CCBHC pioneers and other innovative behavioral health leaders.

