The paperwork that comes with a behavioral health practice can be seen as a necessary evil.
Documenting case notes is not only an important element to charting patient progress, depending on the clinical setting it can be key for reimbursement. But as the requirements for documentation are growing, does the additional administration come at a price?
Why is behavioral health documentation necessary?
The Centers for Medicare and Medicaid Services (CMS) holds all healthcare providers ‘responsible for documenting each patient encounter completely, accurately, and on time.’ It cautions that incomplete or inaccurate documentation could result in unintended or even dangerous outcomes. The many federal and state laws that govern documentation requirements are in essence created for the benefit of consumers and providers alike, with the goal of reducing fraud, waste, and abuse.
As all behavioral health clinicians are potentially subject to an audit of their documentation, the CMS suggests that clinicians conduct regular self-audits to be sure that their documentation is complying to necessary standards. Clearly, the starting point is to implement a solid medical records documentation policy, even if you are in a solo practice. If using an audit tool you should ensure that it covers the documentation policy and coding standards in your specific region.
To conduct a thorough self-audit of your practice, start by designating a staff member to select a random sample of records to review as a ‘spot-check.’ It is important that someone other than the clinician that made the records review them to remove any bias. Practitioners in solo practices might want to partner with another solo practitioner to review each other’s records.
How large is the burden of documentation?
Correctly creating and reviewing medical record documentation places an understandable burden on clinicians. Clinicians spend on average 35% of their time documentation patient data. In real-world terms, clinicians were found to spend an average of 16 minutes and 14 seconds on documentation for every patient encounter.
There has been concern expressed that increased usage of electronic health records would lead to a greater burden of documentation with decreased time for face to face patient care. There is evidence to support this theory. One study found that the implementation of structured and standardized EHR led to a 8.5% decrease in time for face-to-face patient care.
Extra administrative tasks have been shown to divert time and focus from ‘providing actual care to patients’ and may prevent clients from receiving the most appropriate care.
Documentation burden adding to clinician burnout
The negative effects of increased time spent on case documentation is more far-reaching than just limiting the time spent on face to face meetings. Spending more time on administrative tasks and paperwork has been shown to contribute to burnout among behavioral health practitioners.
Burnout has been defined as having three dimensions; a) emotional exhaustion; b) depersonalization and detachment from work and clients; and c) reduced personal accomplishment or a feeling of personal or professional inadequacy as well as reduced productivity and coping skills. The consequences of burnout are profound, including psychological effects such as insomnia and depressive symptoms, as well as a whole host of physical effects, such as coronary heart disease, gastrointestinal issues, and respiratory problems. The toll of burnout in behavioral health clinicians has led some to leave the profession.
Clinician burnout comes at a high cost, both figurative and literal. In addition to the human cost of illness and personal struggle, clinician burnout comes at a financial cost to healthcare systems. If clinicians leave their practice as a result of burnout, new clinicians must be hired in their place with all the associated costs of recruiting and onboarding new staff. With few clinicians available to see patients, healthcare systems stand to lose revenue, and most importantly, the clients themselves lose from the reduction in experienced clinicians.
Studies into burnout in behavioral healthcare practitioners have produced some interesting results. Up to 50% of behavioral health clinicians report moderate to severe burnout. Private practice practitioners were found to have lower levels of burnout and higher levels of job satisfaction than those working in the public sector. This could be in part due to the greater administrative burden placed on some public sector practitioners. Behavioral health practitioners working in the public sector have been characterized as ‘caught in a struggle’ between their responsibilities to their clients and the duties placed upon them by their organization. Indeed the practical requirements of collecting treatment outcomes has been demonstrated to be the biggest deterrent in clinicians collecting them.
Overcoming clinician burnout
The best way to overcome burnout has been the topic of much discussion. Although many things have been discussed from guided imagery to mindfulness practice, the literature points to techniques that bolster clinician resilience as having the greatest impact on burnout and associated compassion fatigue.
However, recovery from burnout is complex. Even when interventions have been implemented, individuals might be resistant to expending the necessary effort to improve their situation. This leads researchers to conclude that avoiding burnout is a more effective strategy.
Streamlining documentation to avoid mental health provider burnout
This can seem easier said than done. The burden placed by case documentation can appear insurmountable. It has been recommended that human resource management should decrease the administrative burden on clinicians. If that is not possible, then administrative healthcare tasks that cannot be eliminated should be regularly reviewed, revised, and streamlined with the goal of minimizing the burden.
Reducing the burden of case documentation is a worthy goal for healthcare systems as a whole. There are measures that individual clinicians or practices can make to reduce the burden, even within the current framework. Recent developments in digital platforms for behavioral health may hold the answer to this challenge.
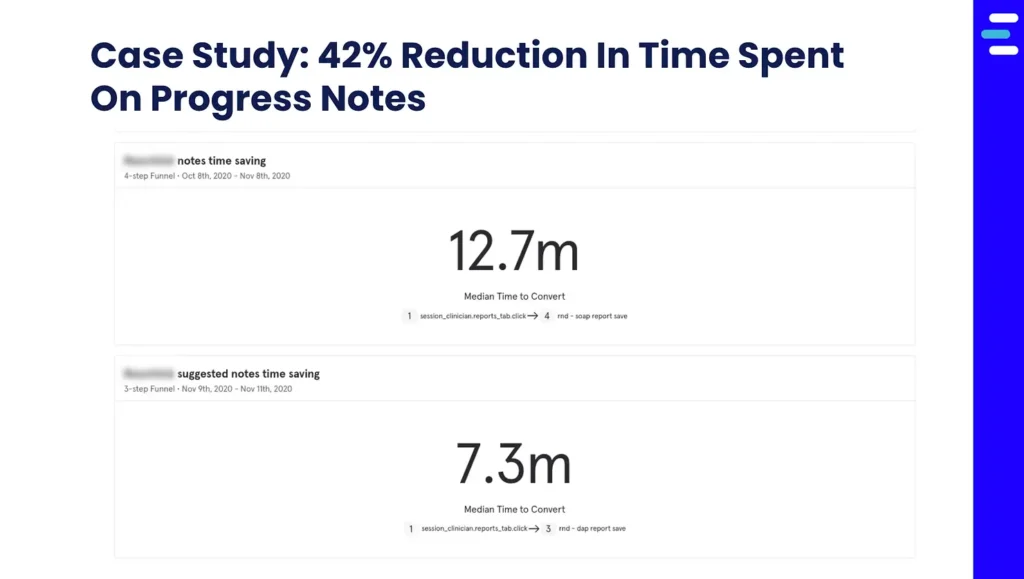
The Eleos Health digital platform was designed as the next generation in workflow support tools for behavioral health clinicians. Using secure therapy-specific voice analysis, Eleos provides clinicians with an automated compliance-ready progress note, while also providing actionable insights into the therapy session. This automatically generated compliance-based baseline for progress notes reduces the time spent on average from 12-15 min per note before Eleos to 6-7 min per note with Eleos.
Eleos also automates the collection of client outcomes, sending relevant tests to clients between sessions. This information is then collated and presented to the clinician on a HIPAA compliant dashboard for easy review and treatment planning. This allows clinicians to practice measurement-based care with ease.
While case documentation is always going to be a part of a behavioral health clinician’s workflow, reducing the weight of the administrative burden is essential for preventing burnout. Thankfully, new digital tools are meeting this challenge for the benefit of behavioral health clinicians and their clients.
