There’s no question that technology-enabled workflows are becoming the norm in behavioral healthcare. Advancements in artificial intelligence and augmented intelligence are driving a shift in how organizations support their workforce while providing new opportunities for providers to improve client care.
But what exactly is augmented intelligence, and how can it be used in behavioral healthcare? In a recent webinar co-hosted with the Texas Council of Community Centers, we explored the concepts of artificial intelligence vs. augmented intelligence technologies in behavioral health, demonstrated how Eleos Health CareOps Automation reduces provider administrative work by 50%, and identified new opportunities to support the Certified Community Behavioral Health Clinic (CCBHC) model of care using this technology.
Artificial Intelligence vs. Augmented Intelligence in Behavioral Healthcare
The term artificial intelligence (AI) was coined in the mid-1950s to describe some of the emerging technologies at that time. AI refers to a computer system that is able to perform tasks normally requiring human intelligence.
Only recently has AI begun to push the limits of healthcare. We’re now seeing the emergence of mature technology that is coming to behavioral healthcare in ways that we have never seen before.
AI can do things that humans can do, but it does them faster and in a variety of different ways. However, AI is not a substitute for human intelligence.
The American Medical Association advocates for use of the term augmented intelligence to represent the types of artificial intelligence that enhance human intelligence, rather than replace it.
In a recent paper, we collaborated with MIT Sloan School of Management and the Center for M2 Health at Palo Alto University, to explore the types of Augmented Intelligence in use across behavioral health today, as well as their benefits and challenges.
We found that in behavioral health, augmented intelligence technologies fall into three categories:
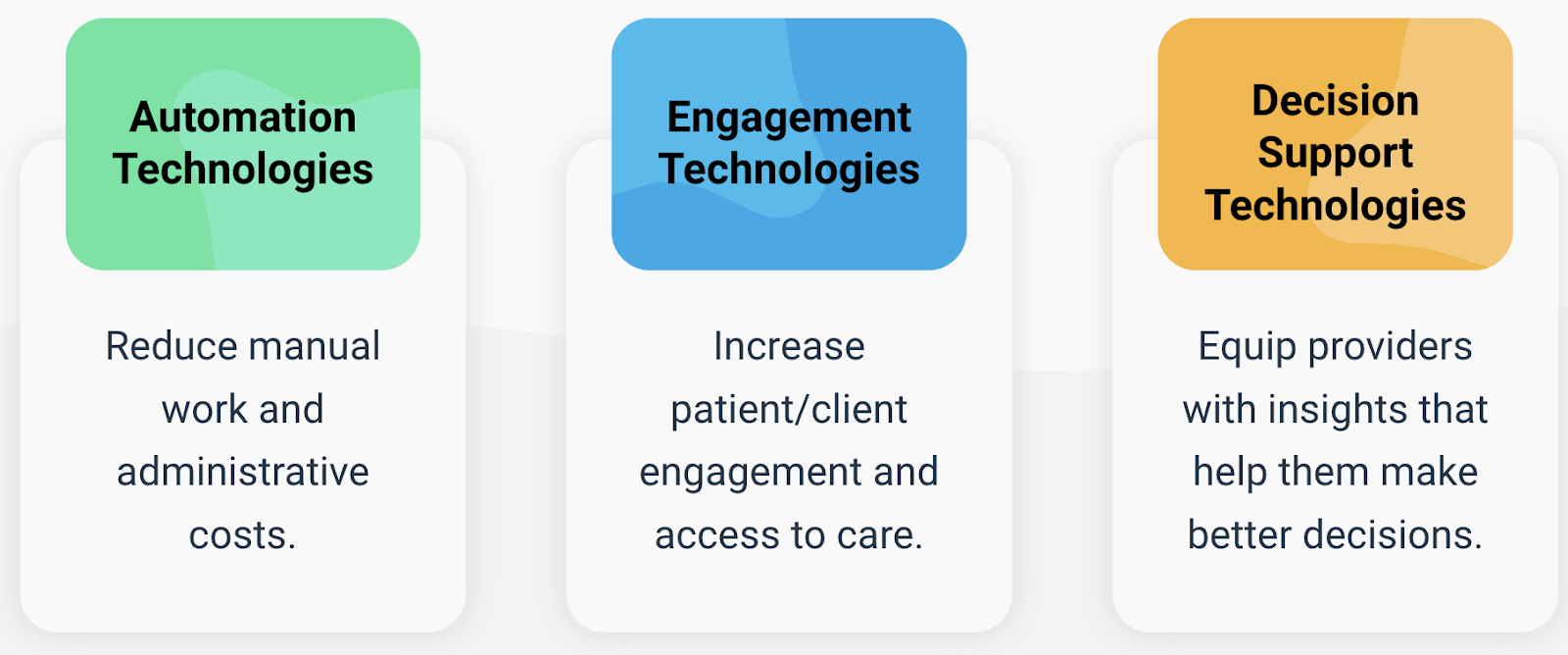
Eleos Health’s capabilities extend across all three areas by assisting providers with progress note documentation and generating objective insights into behavioral health sessions. Providers are using these insights to improve care and they are often sharing the insights with clients in order to improve their engagement and accountability.
Unlocking the Power of Conversation in Behavioral Health
There are several challenges being faced in today’s industry. One of the major challenges is that there are administrative burdens that stand in the way of providing effective care.
In order to document care delivered in accordance with compliance and billing requirements, providers spend over 20% of their available time completing documentation. This is time that could be better allocated to client care.
With approximately 6,000 words spoken during the average 45-minute behavioral health conversation, providers have to rely on memory and manual note taking to capture the relevant details, a process which may take upwards of 10 minutes per individual session and even longer for group sessions. However:
- Only 4% of the conversation is captured in the progress note
- Progress note quality varies and is 100% reliant on the provider’s ability to remember and document details
- Full-time providers see 40-50 clients per week and may take days to complete notes, putting note quality at risk
In addition, providers don’t have an efficient way to obtain objective feedback on their sessions and identify training or development needs on an ongoing basis. For leaders and supervisors, transparency into the quality and consistency of care being delivered is limited.
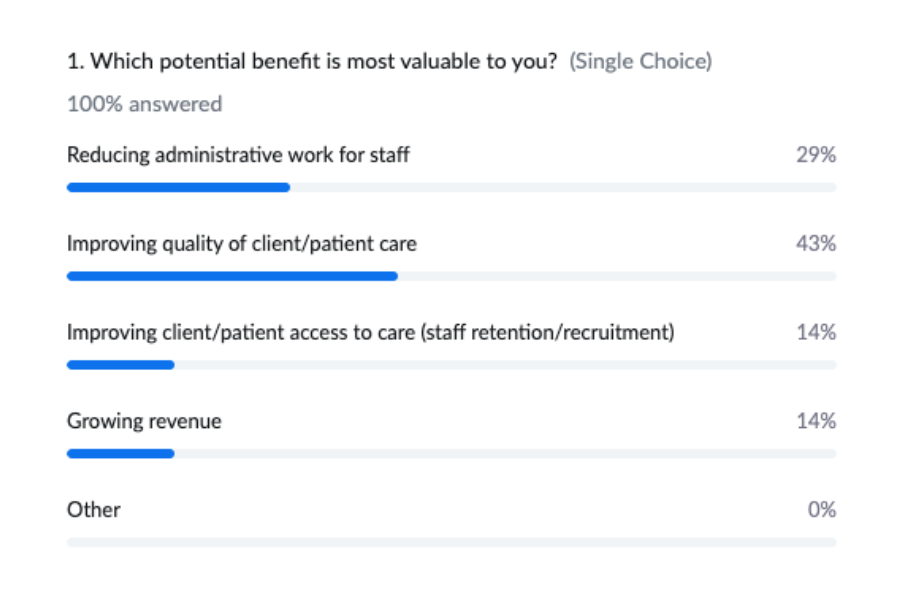
When the live webinar audience was polled on what they perceived to be the top potential benefit of augmented intelligence, improving quality of care and reducing administrative work were at the top of the list.
Understanding Eleos CareOps Automation
The source of Eleos Health’s augmented intelligence is our CareOps Automation platform. CareOps Automation turns behavioral health conversations into documentation and intelligence, improving care and reducing work. The platform consists of three main capabilities today:
Documentation Assistance
Automatically generates over 50% of required documentation for every session so that providers can reduce time spent on administrative work and focus on having conversations instead of taking notes
Session Intelligence
Eye-catching, user-friendly session analytics that show providers evidence-based techniques used, therapeutic alliance indicators, key moments, themes and topics so that they can assess their performance and identify opportunities to improve care
Leadership Reporting
Dashboards that equip supervisors and leaders with unprecedented visibility into staff activity, caseloads and performance as well as key population metrics and trends
Taken together, Eleos CareOps Automation can help organizations to:
- Free providers from ops
- Unlock visibility into care quality
- Scale training and supervision
Customers have achieved upwards of 50% in progress note documentation time savings with most notes being completed within 24 hours. On a leadership level, Eleos CareOps demonstrates how an organization is using evidence-based care and its impact on the population. On average, Eleos customers achieve 30%+ increases in the number of evidence-based techniques used per session per provider, ultimately helping people get better, faster.
Supporting the CCBHC Model of Care

Eleos is a great fit for the CCBHC model of care. The CCBHC compliance criteria supported include:
Cultural Competence and Other Training
Think about how you train staff to meet the CCBHC requirements. Are they using evidence-based care? Are they trained to document it accurately? Eleos provides a great tool to help providers ramp up faster to meet the clinical guidelines of the organization.
Quality and Other Reporting
For quality and reporting, this type of technology allows you to understand whether you’re using evidence-based practice at the session level, at the department level, at the site level, or at the whole network level, and then demonstrate this to stakeholders.
Outpatient Mental Health and Substance Use Services
From a quality assurance perspective, the tool shows that providers are actually providing those services and are accountable for the care that they provide.
Final Thoughts on Augmented Intelligence in Behavioral Health
Our frontline behavioral health providers deserve more.
They want to spend more of their time helping people. They want more opportunities for training and development. They want to deliver the best care possible and be fully present with their clients.
Advances in technology offer new opportunities to support frontline providers and leadership teams. These technologies can help to free providers from operational tasks, unlock visibility into care quality and scale training and supervision.
Eleos Health believes that with less time focused on ops, more becomes possible.
Learn More
Catch the highlights video or watch the full webinar on-demand.
