Imagine getting up at 4 a.m. to finish yesterday’s documentation.
You work on that until 7 a.m., then get ready and head out the door—leaving just enough time to get to your first patient. You’re on the road all day, jumping from visit to visit, barely even taking a break to eat the frozen green beans you packed for lunch. You see patients until 5 or 6 p.m., head home to spend the evening with your family, go to bed, and wake up before the sun to do it all over again.
Yup, you read that right. That’s a 14-hour day (with very few breaks), meeting with families who are going through the most emotional time of their lives. And you’re doing the administrative side of the job during your personal time, because typing up a note while you’re face-to-face with a grieving family just isn’t an option.
That’s the story one hospice nurse with over 9 years of experience told us. Her name is Jennifer.
Unfortunately, her story is not unique. There are thousands of “Jennifers” who need our help, which is why we’re bringing our AI solutions to home health and hospice professionals—and making it our mission to change this heartbreaking reality.
Why Hospice Care Became Her Passion
As a hospice nurse, you’re invited not just into people’s homes, but into their families—at a time that’s incredibly vulnerable and emotional. The job goes beyond simply checking vitals or administering medications. You’re often the person helping a family understand what’s happening and what to expect in the last days of their loved one’s life. In a culture that doesn’t talk openly about death or dying, it’s an especially important role.
Jennifer describes it as a “sacred space.”
That’s what made her passionate about this line of work, and it’s why the administrative burden hits so hard. When clinicians feel rushed, distracted, or depleted, it doesn’t just impact a workflow—it impacts a family’s experience with loss and a patient’s end-of-life care.
“I want to help support those workers and those families who so readily invite us into that sacred space,” said Jennifer, who recently joined the Eleos team. “I want those workers to be able to be present and to serve with their whole hearts in those spaces. This is how I can give back to a field that has given so much to me and forever changed my view of life, living, and death.”
A Day in the Life
In hospice, care happens in the home. And paperwork—apparently—happens at 4 a.m.
For Jennifer, a typical day as a hospice nurse looked like this:
- 4:00 a.m. → Finish documentation from the day before (when her brain could function again).
- 7:00 a.m. → Get ready for the day.
- 8:00 a.m. to 5:00 or 6:00 p.m. → Drive to visits and see patients.
- Evening → Be with family, exercise, and decompress.
- On-call nights → Occasionally cover urgent, late-night visits.
She often avoided charting in people’s homes because of how delicate the face-to-face time is. Opening a laptop and taking notes during those moments changes the entire experience. Plus, in many rural areas (a symptom of the on-the-go aspects of the job), it’s often hard to get reliable internet service anyway.
So instead, she listened. She cared. She took notes where she could, and she finished her documentation later—usually after hours.
That’s where the pressure piled up.
When Death Isn’t the Burnout Driver
Jennifer pointed out something surprising: The constant proximity to death and grief isn’t always what breaks clinicians in hospice care.
“I burned out more than once,” Jennifer shared. “Not because of the exposure to death and dying, but because of the administrative burden and the requirements that were not related to patient care.”
Regardless of your profession, finding meaning and purpose in your work is a huge factor in avoiding burnout. And in hospice, there’s a lot of meaning. For many clinicians, that’s actually what keeps them in the work—not what forces them out.
The passion is snuffed out by the administrative requirements. By the number of patients they’re asked to see in a day. By the hundreds of miles they drive to and from appointments. Combine that with staffing shortages and scheduling constraints, and nurses like Jennifer end up feeling like they can’t spend enough time with the patients and families who need them—stripping away the very meaning that fills their cup.
“I felt like I didn’t have a voice and wasn’t able to truly be present with my patients and families,” said Jennifer. “I felt like I had to rush through my visits just to make sure I could see everyone I needed to, coordinate their care, get my documentation done, and meet my family and home obligations.”
What pushed Jennifer—and so many clinicians she worked alongside—toward burnout was:
- The moral distress of being unable to practice the way they believed was right, and
- The hours of work that bled into their personal lives.
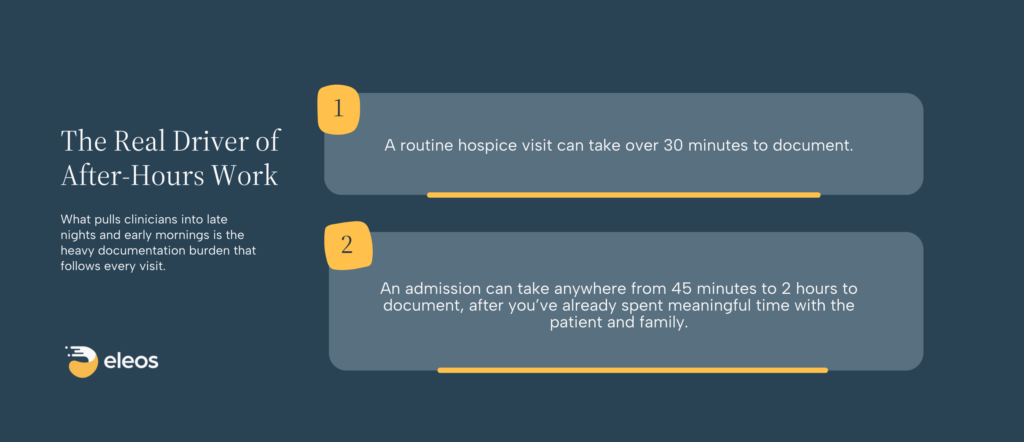
And the biggest source of that after-hours work? The unusually high burden of care at home documentation:
Jennifer reflected on a particular day when she was sent hours away for an admission. She drove two hours, spent two hours with the patient and family, and then faced more hours of post-visit documentation and care coordination. When the office called asking her to take another admission that same day, she couldn’t. It wasn’t physically possible within the workday.
The response she received was familiar to many clinicians: “Just get your documentation done faster.”
And then there were times she was pulled away from a family in distress to respond to another crisis because her organization was so understaffed. Imagine the stress that puts on the patient and the patient’s family. It’s a system that forces impossible tradeoffs.
Documentation Burden Becomes an Organizational Problem
The effects of clinician burnout don’t end with the individual practitioner. They don’t even end with that clinician’s patients. Because when clinicians are buried in documentation and administrative work, it also affects the entire organization’s ability to deliver high-quality care at scale.
The domino effect manifests in very real ways, including:
- Retention and Staffing Stability: Burnout drives turnover. Turnover deepens staffing shortages. Staffing shortages increase workload—and the cycle continues.
- Capacity and Access: When documentation turns a single visit into hours of late-night work, organizations can’t simply “add one more patient,” even when the need is urgent.
- Quality and Compliance: Rushed documentation leads to mistakes, copy-pasting, and more QA/QAPI reviews that pull clinicians back into the paperwork cycle, draining time and focus.
- Patient Experience: Presence is felt. So is distraction. In hospice and home health, relationships are a core part of care. When documentation gets in the way, it is detrimental to the relationship—which inherently drags down the quality of care.
Why We’re Expanding Our Mission
Like many clinicians, Jennifer eventually realized the strain she felt wasn’t just about workload—it was structural. She stepped into health technology roles to better understand the systems shaping care at home and to advocate for the clinicians she had once stood beside in the field.
What quickly became clear is that technology often promised to reduce the burden, only to end up increasing clicks, duplicating work, and pulling clinicians further away from patients instead of giving them time back.
That’s why Eleos felt different.
“When I saw Eleos, it was the first time in my 13 years in the health and human services industry that I really thought, ‘This could actually help,’” Jennifer emphasized.
Our mission has always been to help clinicians stay focused on care instead of paperwork. We’ve built our products alongside behavioral health organizations for over five years, listening closely to clinicians and leaders, measuring impact, and updating our solutions to solve their everyday issues.
Now, we’re bringing that same approach to care at home, because the need is just as urgent.
And Jennifer is at the heart of our care at home team, supporting customers and advocating for solutions that truly make their jobs—and lives—easier.
“I’m here at Eleos to give a voice to the people in similar positions to what I was in, who might not feel like they have one or that their voice is heard,” Jennifer explained. “I want to advocate for them and for this field that is my true love and passion.”
Giving Clinicians Time Back
The first way Eleos helps clinicians in the care at home space is simple: Time. With AI that captures nuanced conversations and turns them into clear documentation in minutes, clinicians can finish their notes 70% faster without sacrificing quality.
That means:
- No more 4 a.m. documentation sessions;
- Fewer evenings spent charting instead of resting or being with family; and
- More energy and attention for patient care during visits.
“My goal is to help lift that documentation burden so that care at home workers can give themselves to their work and to their home lives,” Jennifer explained. “So that they can be fully present in both spaces and not have to sacrifice one for the other.”
Improving Compliance & Care Quality
Time saved isn’t the only benefit of Eleos. Our platform is designed to meet the complex regulatory requirements that come with care at home documentation, including standardized assessments and quality measures like:
- OASIS-E
- HOPE
- Advance Care Planning (ACP) and Palliative Quality Measures (QMs)
With dynamic, discipline-specific forms that automatically adapt based on service type, client population, and clinician role, the system recognizes whether a clinician is completing an OASIS-E assessment, a HOPE form, or a palliative symptom scale—and tailors the workflow accordingly.
To further reduce friction, our AI-powered compliance solution, Eleos Compliance:
- Scans 100% of notes automatically for compliance risks;
- Flags issues like cloned content, missing interventions, or disconnected action plans; and
- Surfaces gaps before notes are finalized—rather than days or weeks later.
Instead of manually auditing just 5–10% of documentation, QA/QAPI teams can check every note and focus their attention only where it matters most. Clinicians aren’t pulled back into “finished” work, and organizations reduce the risk of audit fails or avoidable clawbacks.
Supporting Care at Home
Ultimately, these benefits go beyond helping clinicians on a personal level.
By reducing documentation time while improving note quality, Eleos helps care at home organizations:
- Stabilize their workforce by addressing a major driver of burnout;
- Increase capacity without stretching clinicians further;
- Improve documentation timeliness and prevent revenue cycle delays; and
- Deliver more consistent, higher-quality patient care.
What “Better” Should Look Like
No hospice care worker should burn out because of paperwork. If someone has the heart to serve patients and families in their most vulnerable moments, the systems around them should make that work easier, not harder.
A better future for care at home is one with more time and less after-hours admin work for those on the front lines.
As Jennifer put it during our conversation, “Technology like Eleos helps make care providers, care providers again.”
Taking the documentation and compliance burdens off their shoulders allows them to be more present and feel more fulfilled in the work they set out to do.
That’s the future we’re working toward at Eleos. One where clinicians can build meaningful, sustainable careers, organizations can deliver high-quality care at scale, and technology finally does what it always promised to do: Support the people at the heart of care.
If that sounds like the future your organization is working toward, too, schedule some time to chat with us.

